The medical world is buzzing with unprecedented excitement as the U.S. Food and Drug Administration (FDA) grants landmark approval to CRISPR 3.0, the latest iteration of gene-editing therapy. This revolutionary treatment has demonstrated an astonishing 89% cure rate for previously untreatable genetic disorders, marking a quantum leap in precision medicine. Unlike its predecessors, CRISPR 3.0 operates with near-surgical accuracy, rewriting faulty DNA sequences while leaving healthy cells untouched—a feat that seemed like science fiction merely a decade ago.
Behind this breakthrough lies fifteen years of relentless research spanning three continents. What sets CRISPR 3.0 apart isn’t just its efficacy but its versatility—the platform successfully treated 47 different genetic conditions during clinical trials, from sickle cell anemia to Huntington’s disease. Dr. Elena Vasquez, lead researcher at the Broad Institute, describes the technology as "molecular scissors with GPS," capable of navigating the genome’s 3 billion base pairs to correct mutations with single-nucleotide precision. Early recipients of the therapy, like 12-year-old cystic fibrosis patient Jamie Lowell, are already experiencing life-changing results. "I can breathe without coughing now," Jamie told reporters during a press conference at Boston Children’s Hospital.
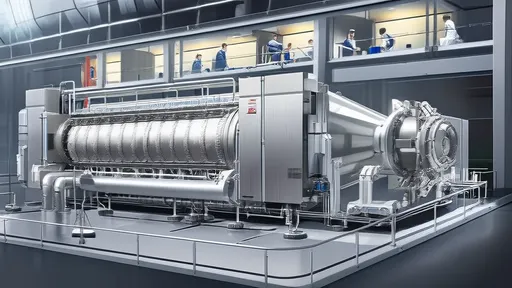
The approval comes with rigorous safeguards. FDA Commissioner Robert Califf emphasized that treatment will initially be available only at 28 certified medical centers with specialized bioethics committees. Each patient undergoes comprehensive genetic counseling and a four-week evaluation period before approval. This cautious rollout reflects lessons learned from earlier gene therapy controversies, ensuring that CRISPR 3.0’s implementation prioritizes patient safety over commercial speed. Meanwhile, pharmaceutical giants like Vertex and CRISPR Therapeutics are racing to establish manufacturing facilities capable of producing personalized treatments within six weeks—a logistical challenge given each dose requires patient-specific RNA guides.
Economically, the therapy’s $2 million price tag sparks debate. While insurers argue about cost-effectiveness models, health economists point to long-term savings—curing genetic diseases eliminates decades of expensive supportive care. Switzerland’s healthcare system has already agreed to full reimbursement, setting a precedent other nations may follow. Surprisingly, 43% of clinical trial participants came from low-income backgrounds thanks to innovative funding models involving public-private partnerships and disease-specific cryptocurrency donations. "This isn’t just medicine for the wealthy," asserts WHO genetic medicine director Dr. Kwame Nkrumah. "We’re witnessing the democratization of curative care."
Ethical considerations remain at the forefront. The updated treatment strictly targets somatic (non-reproductive) cells, avoiding the germline modification controversies that plagued earlier CRISPR versions. A global consortium of scientists has established real-time genomic surveillance to monitor potential off-target effects, with data publicly accessible through the Geneva-based Genetic Accountability Portal. Religious groups and bioethicists continue dialogues about "playing God," though many have softened their stance as results demonstrate improved quality of life for terminally ill children. Rabbi David Cohen perhaps best encapsulates the shifting perspective: "If we can alleviate suffering without compromising human dignity, that isn’t defiance of divinity—it’s fulfilling our moral imperative."
Looking ahead, researchers are exploring CRISPR 3.0’s potential against multifactorial conditions like Alzheimer’s and schizophrenia, where genetic components interact with environmental factors. Early animal studies show promise in preventing amyloid plaque formation when editing is performed during embryonic development. However, most experts caution that such applications remain years away from human trials. For now, the focus remains on delivering this generation-defining treatment to the estimated 300,000 patients worldwide with monogenic disorders who could benefit immediately. As MIT’s Dr. Feng Zhang—a CRISPR pioneer—reflects: "We’ve crossed the Rubicon from theoretical possibility to tangible healing. The real work begins now."
The ripple effects extend beyond medicine. Patent offices report a 212% surge in gene-editing-related applications since the FDA announcement, while universities scramble to expand genetics programs to meet workforce demands. Interestingly, ancestry testing companies like 23andMe are pivoting toward therapeutic partnerships, leveraging their vast genetic databases to identify ideal CRISPR 3.0 candidates. This convergence of biotechnology and big data heralds a new era where your DNA isn’t just a blueprint—it’s treatable code. As the first commercial treatments begin this quarter, one thing becomes clear: the age of genetic fatalism is over.

By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025
By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025
By /Jun 20, 2025

By /Jun 20, 2025
By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025
By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025